I thought the expense of having a baby would come after conception.
Turns out – I’m wrong.
Cost of Assisted Reproductive Technology
For those of us struggling to get pregnant, sticker shock hits even before we get a positive pregnancy test. Many of us head to an infertility clinic in the hopes of getting pregnant. But the exorbitant price tag on technological procedures make having a baby seem out of reach – even for those of us with insurance.
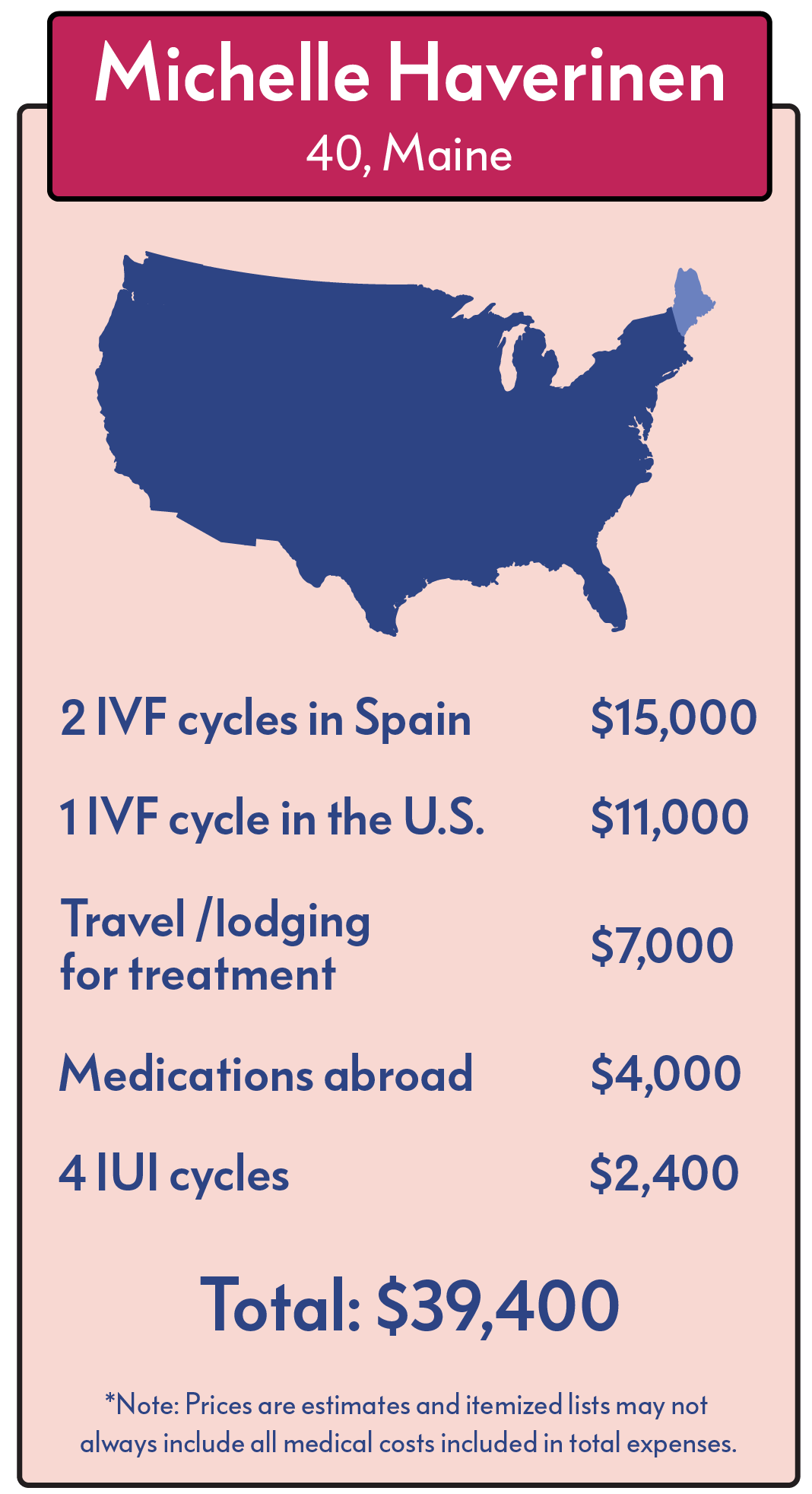
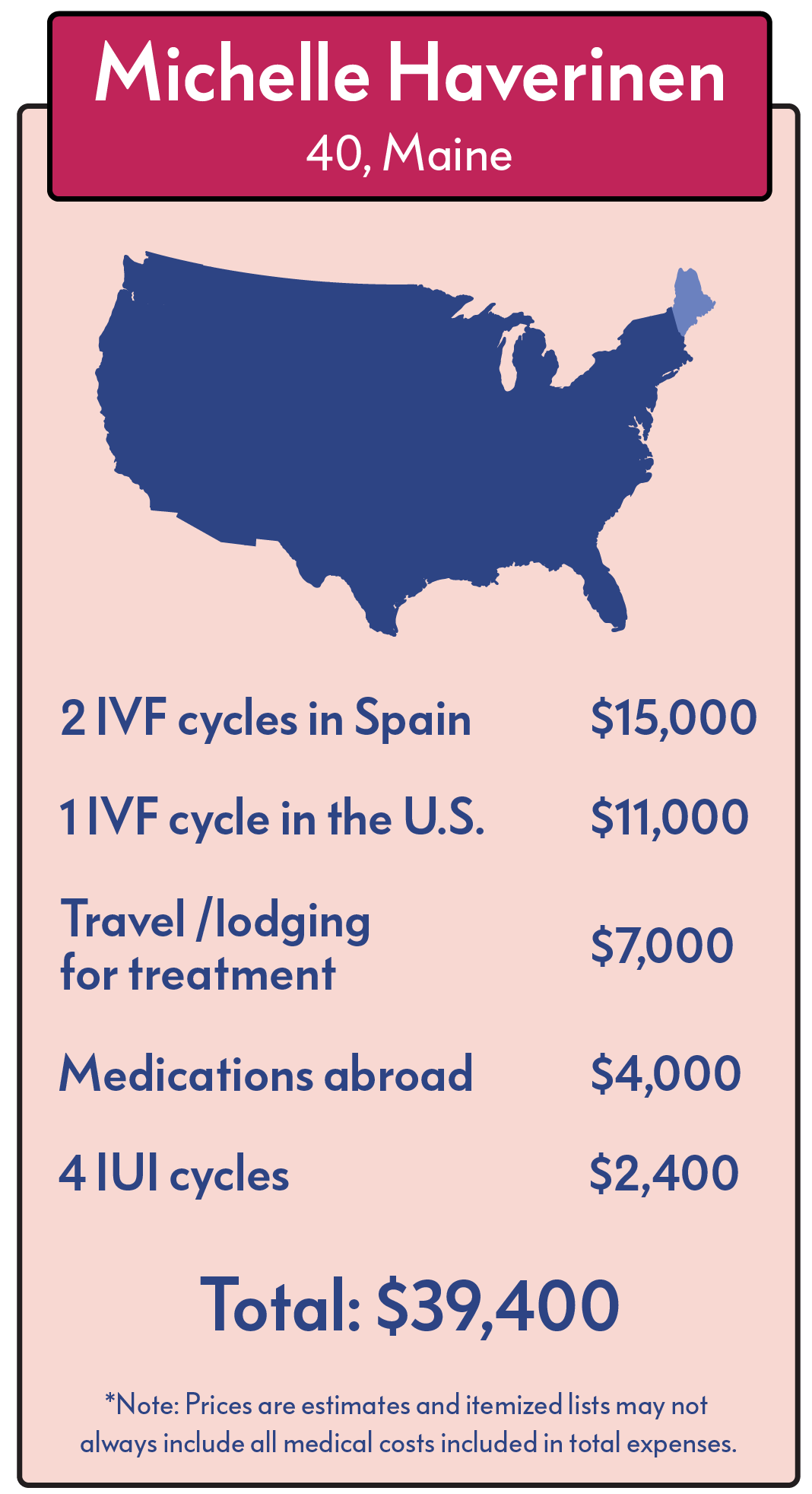
According to RESOLVE, an infertility patient advocacy organization, most insurance policies don’t cover most assisted reproductive technologies. So when you’re struggling with infertility and you go to your doctor for help, you’ll probably need to have your wallet ready. The average costs of infertility treatments look like this (1):
IUI cycle: $865
IVF cycle using fresh embryos (not including medications): $8,158
IVF Medications: $4,000
Average additional cost of ICSI procedure: $1,544
Average additional cost of PGD procedure: $3,550
Who has $12,158 to hand over to give IVF a try?
Not too many people, which is why infertile couples often take out loans to finance their hope of having a child. Some can afford only one attempt and others have to turn away before the first consultation.
Fortunately, banks, institutions and some clinics have developed financing programs specifically for infertility and a few organizations are awarding infertility scholarships. This is a good start but not everyone is in a position to take out a loan – especially in today’s economy – and the winners of scholarships are limited to just a few couples.
So the decisive factor for many infertile couples is money.
Unfair? Yes. Wrong? Absolutely.
But that’s the reality right now: in the US there are only fourteen states that currently have laws that require insurers to either cover or offer to cover some form of infertility diagnosis and treatment (2). And within those states self-insuring businesses do not have to implement these regulations at all (3).
Throw into this difficult situation an economic crisis that caused the loss of 2.6 million jobs in 2008 (the worst year since 1945) with many more fearing the loss of their income this year. It’s not a bright picture but there is a bright side for those of us suffering from infertility and willing to try something else: natural infertility treatments.
Fertility Treatments – Free and Effective
Many natural fertility treatments are not only proving to be effective but they are also considerably cheaper than assisted reproductive technology – costing near next to nothing.
Diet and exercise are two of the most thoroughly researched – and cheapest – natural fertility treatments.
Dr. Jeremy Groll, an expert in fertility treatment and author of Fertility Foods, noticed the effectiveness of diet with one of his patients who had been trying to conceive for two years with an irregular cycle. He had her change her diet and, after two months, she lost eight pounds and achieved a successful pregnancy. This was just the beginning though; he has since gone on to help countless women realize their dream of having children with his diet and exercise program that is, “low-cost, painless and free of detrimental side effects” (4).
Published research results are also beginning to pile up in support of effective and free natural fertility treatments.
In 2007, scientists reviewed published research on the effect lifestyle factors have on reproductive health (5). They concluded from the evidence that a program to encourage and facilitate the necessary lifestyle changes will improve couples’ chances of successful pregnancies, “minimizing the need for costly and invasive infertility treatment.” More studies are needed on the effects of lifestyle on fertility but there was enough evidence to support the recommendation of a lifestyle intervention program that includes exercise, a healthy diet, no smoking, caffeine reduction and stress reduction.
A group of researchers from Australia went as far as conducting a cost savings analysis of a weight loss program for obese infertile women (in Australian dollars) (6). Their results show that weight loss results in improvement of reproductive outcome for all forms of fertility treatments and costs considerably less.
Before the program, 67 women had two live births with infertility treatment costs totaling A$ 550,000, a cost of A$ 275,000 per baby. The same women went through a 6 month weight loss program (losing an average of 10 kg or 22 pounds) which resulted in 45 babies (18 of the pregnancies were spontaneous, i.e. natural) and A$ 210,000 worth of treatments, a cost of A$ 4,600 per baby. This shows that weight loss is very effective in boosting fertility and much cheaper with a savings of A$ 270,400 (or over US$ 180,000) per child.
Let’s not pretend like weight loss is easy but, this study shows that with support and the right diet, it can lead to a priceless reward.
There are other inexpensive and effective natural fertility treatments other than just diet and exercise. I’ll be covering them in detail on a naturally getting pregnant page soon (there’s that ‘s’ word again). But right now my stomach is grumbling for a snack, so I’m going to go eat something healthy and improve my fertility without having to break the piggy bank.
 I find myself here…again.
I find myself here…again.

 Halfway through my second pregnancy, I had little hope that the vomiting would end. My first pregnancy was worse, vomiting in excess of eight times a day. I was 20 weeks along in my second pregnancy and we had already resolved that this would be the last child for us. I was too sick to care for my two year old full time and I could barely manage a simple daily routine. Since I was sick until the day of delivery with my first daughter, I had given in to the idea of about 20 more weeks of continued illness.
Halfway through my second pregnancy, I had little hope that the vomiting would end. My first pregnancy was worse, vomiting in excess of eight times a day. I was 20 weeks along in my second pregnancy and we had already resolved that this would be the last child for us. I was too sick to care for my two year old full time and I could barely manage a simple daily routine. Since I was sick until the day of delivery with my first daughter, I had given in to the idea of about 20 more weeks of continued illness.


 I was at the dentist this week.
I was at the dentist this week.